Psoriatic Arthritis (PsA)
- What is it?
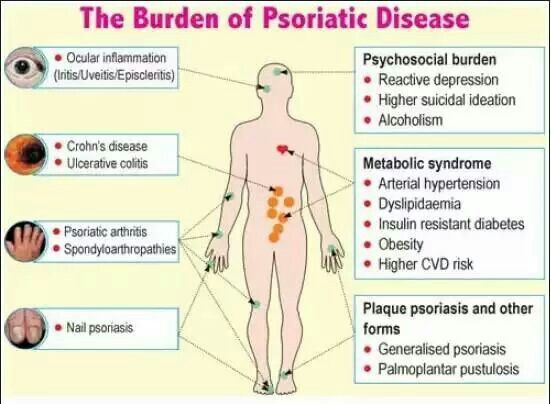
- Psoriatic arthritis occurs when your body’s immune system begins to attack healthy cells and tissue. The abnormal immune response causes inflammation in your joints as well as overproduction of skin cells. Psoriatic arthritis is a form of arthritis that affects some people who have psoriasis. Most people develop psoriasis first and are later diagnosed with psoriatic arthritis, but the joint problems can sometimes begin before skin lesions appear.
- Symptoms
- Psoriatic Arthritis sometimes mimic that of Rheumatoid Arthritis (RA) however there are some mild differences that lead to the diagnosis of PsA opposed to RA which includes but not limited to the following:
- Psoriasis lesions
- Swollen fingers and toes at are painful and sausage-like
- Foot pain. at the points where tendons and ligaments attach to your bones — especially at the back of your heel (Achilles tendinitis) or in the sole of your foot (plantar fasciitis).
- Lower back pain. Resulting in spondylitis.
- How is it diagnosed?
- The diagnosis of PsA may include use of images i.e. x-rays or MRI, labs test and physician exam findings such as joint exam, exam of fingernails for pitting, flaking and other abnormalities and pressing on the soles of your feet and around your heels to find tender areas.
- Psoriatic Arthritis sometimes mimic that of Rheumatoid Arthritis (RA) however there are some mild differences that lead to the diagnosis of PsA opposed to RA which includes but not limited to the following:
- How is it treated?
- Now cure exist for PsA however those diagnosis with this disease have a wide range of treatment options that can be taken to help control symptoms. Some treatment that may be prescribed NSAIDS (Nonsteroidal anti-inflammatory drugs) such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others); Steroids such as prednisone, or high doses of steroids such as methylprednisolone (A-Methapred, Medrol) for more severe cases; Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate (Trexall, Otrexup, Rasuvo), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine); include azathioprine (Imuran, Azasan) and cyclosporine (Gengraf, Neoral, Sandimmune); TNF-alpha inhibitors include etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), golimumab (Simponi) and certolizumab (Cimzia); and Newer medications include apremilast (Otezla), ustekinumab (Stelara) and secukinumab (Cosentyx).
- Joint replacement and steroid injections are also other alternatives as well.